William Hayes-Wood
Observer of life from a sedentary position
WHWood555@aol.com
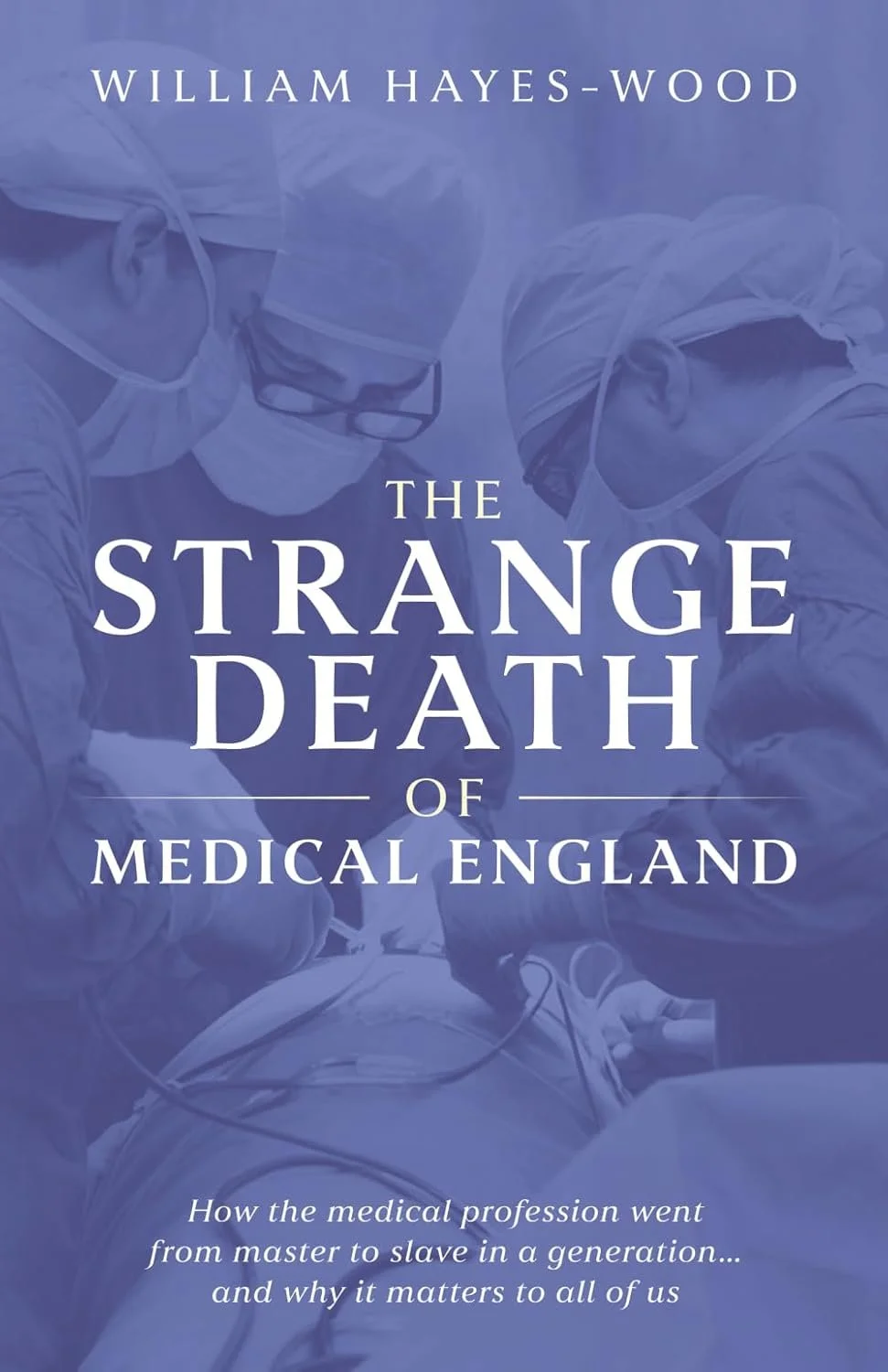
The Strange Death of Medical England by William Hayes-Wood
Amazon reviews:
“Fantastic book, very accessible even to non-medical readers. Cuts to the heart of the matter with the disgruntlement of today’s doctors at the political forces behind the morphing of the NHS”.
“Well-written, relevant and informative. This book is written by an experienced senior surgeon with insight, knowledge and with patients at its heart. Highly recommended!”
“It’s well worth reading; a good (and for me, recognisable) summary of how we got to where we are now”.
“This concise and very informative book describes, with considerable accuracy, the changes in the medical profession - and indeed the NHS - over the years, that led to the situation we are in in 2025. Mr. Hayes-Wood gives an excellent account of the salient changes, all of which (as a retired NHS surgeon) I remember well. These include the Griffiths report and the introduction of an army of managers and the purchaser-provider system under Thatcher, private finance initiatives under Blair, utter confusion when Andrew Lansley was Health Secretary and the 'centralisation' of recruitment for medical training, disliked by so many of our young doctors. Mr. Hayes-Wood argues convincingly that the sum effect of these changes, by design, has resulted in the death of medicine as an independent profession. He concludes that the provision of healthcare in England has come 'full circle' to a situation that existed prior to the inception of the NHS, with increasing private involvement and, effectively, a 'two tier' service.
Overall, a very good and most readable short book and highly recommended for both the medical profession and, indeed, anyone interested in healthcare and the NHS.”
“As a retired GP who qualified in 1987 I am in complete agreement with William as to how medicine as a profession has been destroyed. Should be compulsory reading for everyone who lives in England”.
AMAZON £7-99
Book Review
CRITICAL
Author: Dr Julia Grace Patterson
Publisher: Harper Collins 2024 £9-99
In her book Critical Dr Patterson champions the National Health Service with uncommon vigour and passion. That is, the National Health Service as originally conceived. Dr Patterson points out, however, that the NHS has been poorly served by the successive governments who have been its custodians so that our health service today falls significantly short of fulfilling its originally stated mission.
Dr Patterson is someone with first hand experience of the hospital system as a young doctor. She has personally had to deal with the serious and ever worsening shortcomings of the system as they have affected both patients and staff in recent years. She paints a vivid picture of life within the NHS. Her description of what it was like for hospital staff during the Covid crisis – when staff were effectively thrown to the wolves by the government – is truly harrowing. Dr Patterson details how successive governments have failed the service and concludes with her own prescription as to how things might be put right. One thing which Dr Patterson is aware of – something that many of her generation may not always appreciate – is that the problems evident today date back to a political decision made forty years ago, before she was even born. A political strategy wilfully – and largely surreptitiously – perpetuated by governments of both colours ever since. So concerned was Dr Patterson that she chose to give up her work to campaign full time in support of the NHS. She set up, with colleagues, an organisation called EveryDoctor to campaign to save the NHS. This book forms an important part of that campaign.
Dr Patterson refers to the founding charter of the NHS and how, in its early years, politicians strove to uphold the charter despite very real financial constraints. She explains how over the past 40 years successive governments have incrementally, repeatedly ignored the founding precepts of the service. This is most evident in a lack of investment so that the provision of services to patients is no longer adequate. Hence the ever lengthening waiting lists for hospital appointments and treatment and the near impossibility of getting a GP appointment in some areas. Dr Patterson concentrates specifically on the harmful impact of the policies of successive governments on patient care. She also touches relatively briefly on the pernicious effect of these policies on staff working within the NHS. The failure of their salaries to keep pace with inflation, the incomprehensible muddle into which the training of young doctors has degenerated and the resulting collapse in morale culminating in strike action. In my view Dr Patterson lets off too lightly the culpability of the medical profession itself in the unfolding disaster and the malign effect of the General Medical Council (now the government’s poodle - or perhaps, more accurately - Rottweiler). But Dr Patterson’s emphasis throughout is centred on patients. On the poor – and deteriorating – quality of service which the NHS is providing for patients, in terms of the quality and convenience of care provided to them; the physical inadequacies of much hospital accommodation; the inefficiencies of many of the IT systems meant to facilitate their treatment; the lack of investment and the half-hearted approach that successive governments have demonstrated in abiding by the founding constitution of the NHS. The creeping privatisation of so many aspects of NHS healthcare is something which Dr Patterson warns is especially destructive, its fundamental role being to divert money into the pockets of private investors rather than into patient care.
The final chapter in Dr Patterson's book proposes her solution to the problems which she has so painstakingly described. In simple terms she is arguing for a mass campaign to bring these issues better to the attention of the general public – that is, the electorate - in order to put pressure on our politicians to redress the balance and return our health service to what it used to be. What it was always meant to be. Her conviction is that – if only the public and medical profession were to bring sufficient clout to bear on the government – verbalise and publicise their dissatisfaction more vigorously and effectively - the government would be compelled to acknowledge the errors of its ways, relent and provide the necessary support and investment to return the NHS to what it should be.
While I congratulate Dr Patterson on her achievement in writing this book, in particular her easy style and her ability to convey the reality of the experience of the NHS for patients and staff today, I am not convinced the endeavour takes us much further forward in finding a realistic solution to the problems described. To fall back on a well-worn cliche - the main comment I have about Dr Patterson's book is that it is the issues she does not discuss, rather than those she does discuss, which are the key to the matter. I am unclear why Dr Patterson chose to set up a new campaigning group – EveryDoctor – when several similar groups were already well established. The one which most closely mirrors EveryDoctor is Doctors for the NHS so I am puzzled why Dr Patterson did not chose to combine resources, offering her obvious talent and enthusiasm to that organisation.
Something I find surprising given the criticisms which Dr Patterson makes of the way the health service has been undermined by successive governments is that nowhere in the book do we find the words neoliberal or neoliberalism. Yet the deficiencies Dr Patterson describes boil down to the all pervading doctrine of neoliberalism which corrupts all aspects of our society today and which every major political party regards as the Holy Grail. My point is that the measures which Dr Patterson espouses to put right the many and obvious failings in the health service can never be adopted in our neoliberal system. Because they fundamentally conflict with neoliberal dogma. A neoliberal government knows no shame and thus cannot be shamed into doing the right thing. (As we have seen most recently in respect of the genocide in Gaza – a different discussion for another day, but no less important for that).
The Labour MP Clive Lewis put it succinctly when he said “My party would not create the NHS” today. He is absolutely right. More to the point, none of the major parties would create the NHS today. Neither the present government nor recent governments for some years past have the slightest interest in the sort of health service which Nye Bevan set up in 1948. Dr Patterson’s plea to campaign to wake up the government is thus bound to fail. Quite simply because the government does not want the NHS to succeed in its traditional format. The government’s interest lies in the entirely opposite direction.
The other reason why I am sceptical about the effectiveness of Dr Patterson's proposed remedy is because - in my long experience - public protest and campaigning, even when well organised and vocal, rarely has any substantial effect on government. The best example of this was the march in protest against the imminent Iraq war, through London in 2003, in which I was proud to take part. The demonstration was absolutely massive in scale. In addition, opinion polling showed that the great majority of the population were against the war and there were some magnificent speeches made both inside parliament and without. But what effect did all this have? Absolutely none. No effect on the government whatsoever. We went to war and the predicted disaster duly ensued.
The government does not respond to public protest. It prides itself otherwise. The government is responsive to the billionaire oligarchs who control that same government, control other governments, control the world economy and control much of the media. It is not responsive to the electorate. As Nietzsche said “the purpose of democracy is not to distribute power; rather its purpose is to legitimise the concentration of power in the hands of the few”. Thus I believe that even a campaign as well organised as Dr Patterson's is, I fear, doomed to failure no matter how unfair this may seem.
If Dr Patterson's prescription is not going to be effective how do we put the situation right? Returning to the sort of health service which we had several generations ago is going to be inordinately difficult. But if the service is going to be saved I do not believe it will come from protests by healthcare workers and mobilisation of large sections of the population. I believe it will only come from a political party which separates itself from the wholly dominant political ethos of neoliberalism and gains sufficient traction in Westminster to get its hands on the real levers of power. I cannot see this ever arising from the three traditional political parties. Whether a new party comes into being with a more humane political and economic philosophy remains to be seen. A party which is prepared to do the right thing for the NHS and the people of this country. For this is the only mechanism that I can foresee which stands a chance of returning to an NHS as originally envisaged. An NHS which Dr Patterson and I - together with so many others – believe this country and its citizens so rightly deserve.
If the government won’t listen then it must be replaced with one which will. Not an easy task but one which may be ultimately achievable, if not in my lifetime then hopefully within the lifetime of young doctors such as Dr Julia Grace Patterson.
William Hayes-Wood
December 2025
Doctors’ Strike vs Miners’ Strike: Disturbing Parallels?
I feel I have a particular connection with these two events. I refer to the current industrial action by resident doctors and the great miners’ strike of 1984-85.
My connection with the former is that I was a practising doctor myself for well over 40 years so have, perhaps, a reasonable understanding of what it is like to work as a doctor in the NHS. As for the miner’s strike, I worked as a senior registrar in South Yorkshire, the heartlands of the strike, while it was going on and became notorious amongst colleagues for arranging for the miners’ leader - Arthur Scargill, bete noire of the establishment – to meet and talk with medical colleagues. I have witnessed at first hand the effects of the industrial action on the miners themselves, on their families and the communities from which they come.
The most frightening parallel between the two disputes is one which may be too disturbing for the young doctor of today to contemplate and one which the young miner of 40 years ago never really believed was realistically possible. That the government of the day – in effect the employer of the doctors and the erstwhile employer of the miners – is not, and was not, actually interested in settling the dispute. The government does not want negotiation. What the government wanted 40 years ago with respect to the miners was to secure a final victory over a group of workers which it had long believed were hostile to government policy, disruptive and a general pain-in-the-arse. The government prepared itself well, over a number of years and – at a time of its choosing, provoked the strike – and defeated the miners game, set and match. Thus there is no coal mining industry – at least nothing worthy of the name – in the UK today.
The present government – and recent governments of both colours - view doctors pretty much as Thatcher viewed the miners in the 1980s. As a special interest group opposed to government policy (in this case as regards government plans for the health service) who are more trouble than they are worth. Just as Thatcher prepared her battle well by building up massive stocks of coal, recent governments have continued to develop the concept of doctor substitutes. Physcian Assistants, Advanced Clinical Practitioners and so on who are used to fill doctor’s jobs. Patients see these non-doctors with increasing frequency and, for the most part, have no idea they’re being seen by someone who is not medically qualified. But, just like the Thatcher government, the present government knows exactly what it’s doing.
Another parallel between the two strikes is the fundamental reason underlying the action. The miners were fundamentally worried about job security. The closure of many pits which was imminent would result in considerable job losses for miners with little prospect of obtaining alternative employment in the economic climate of the day. Although the BMA has somewhat clumsily appeared to focus the current doctors’ action on pay, the real concern is over training and job security. If that were sorted out, the pay issue would be rather less of an immediate concern. The situation regarding medical training and employment in the UK has become catastrophic. We are in the ridiculous situation of our Medical Schools turning out thousands of new doctors every year but no jobs for them within a couple of years of graduation.
Just as the Thatcher government wanted rid of the miners our present government wants rid of the doctors. Both governments view, or viewed, the groups as political obstacles. Of course, the present government would dismiss the allegation as nonsense… just as did the Thatcher government 40 years ago with respect to the miners. But, as the old political adage says “never accept the proposition as the truth until its officially denied”.
Any resident doctor who reads this short article, and manages to reach the end of it, must feel even more depressed than they were at the beginning. The fact is – you cannot negotiate in a meaningful fashion with an employer who does not want to negotiate. This is why I believe the current action is, I’m very sorry to say, doomed to failure. I’m not sure that resident doctors, as a group, fully appreciate this. The BMA certainly does not appear to. I’m not saying the situation is hopeless but I do not believe the upcoming doctors’ strikes are going to do anything positive for the cause. If the medical profession wants to survive and prosper then a fundamental and very serious rethink will be necessary on the part of those who – purport to - lead it.
William Hayes-Wood
December 2025.
Thinking the Unthinkable?
Since publishing my little book The Strange Death of Medical England earlier in the year I have received a considerable amount of feedback. I have discussed and thought about the issues involved a great deal further; these issues being, of course, the state of the NHS, the medical profession and the relationship between the two. At the conclusion of the book I was pessimistic about the future, as I foresaw it, but I did think there was a glimmer of hope. Hope that, even at this late stage, if the medical profession of today finally got its act together and public protest were vigorously mobilised the downwards slide might be at least halted if not reversed. Six months after publication of my book I am much less confident that this is case. My advice to my erstwhile colleagues in the medical profession is that we have reached the stage whereby the only reasonable fall-back position is to think the unthinkable; it may well be time to move on. Sadly, the party, as far as the medical profession is concerned, may well be over.
Governments of both colours over many years past and any government we are likely to have in the future – have worked, and are working - towards a fundamentally different NHS to that we have known since its inception in 1948. No government past, present or future will state openly that this is their plan for fear of public backlash. But all the evidence points inexorably in this direction. As for thinking the unthinkable – it is not a matter of accepting the government is right – I do not believe the government is right. It is a matter of accepting the reality of the situation. It isn’t that what worked in 1948 at the inception of the NHS does not work today. It is that the will of government to make the NHS work in its original format – so evident in 1948 – has long ago evaporated. Not a matter of right and wrong but a matter of politics.
The fundamental change in government philosophy began with Thatcher 40 years ago. The juggernaut has rolled on ever since then, slowly, but relentlessly.
The key to the success of the nascent NHS in 1948 was securing the cooperation of the medical profession. This was essential. If the doctors were not on board the whole project was a non-starter. Initially apprehensive, the doctors’ assent was achieved through the considerable political skill of health minister Aneurin Bevan. Indeed, so successful was Bevan that it wasn’t long before an initially hostile medical profession became one of the strongest advocates of the NHS. In those days it was very much “the doctors’ NHS”. By this I mean the NHS was introduced primarily to facilitate the relationship between doctor and patient. Doctors were to go on examining, diagnosing and treating patients with the government providing the facilities for the encounter and footing an agreed bill. Importantly, the patient paid nothing at the point of contact. Everyone was happy. At first. Even the doctors. In retrospect, you might fairly say Bevan’s NHS Act nationalised the medical profession though it is unlikely that anyone on either side thought of it that way at the time.
It wasn’t long however before the government began to realise that the new health service was costing more to run than it had envisaged. As time went by successive administrations became increasingly concerned with the cost of the NHS but it was not til the Thatcher government in the 1980s that there was a radical re think of the whole scheme. Could the country actually afford the sort of NHS as originally envisaged? Could we go on like this? Thatcher thought not and her neoliberal philosophy has dominated governments of both persuasions ever since.
So how is this juggernaut going to continue to roll forward? So how do I predict that healthcare will be organised in the UK – or more accurately in England – in 25 years from now? How will this impact on patient care and what are the implications for the medical profession?
In stark contrast to 1948 the medical profession is no longer regarded as essential to running the NHS today. It is regarded as one option. Increasingly, other options than doctors – potentially less troublesome, more malleable and cheaper - are seen to be available. Indeed these options have been stealthily developed by government over time with the express purpose of providing another option. I predict that in the future in both primary and secondary care the first port of call for NHS patients will not be a qualified doctor but to something akin to the PA, ACP or ANP of today. The role of these para-medical practitioners will likely be expanded, with greater clinical autonomy, so that they are free to prescribe medicines and order x-rays, scans and so on. There will be much greater use of AI in diagnosis and formulating treatment plans. There will still be traditional medical professionals in the Brave New NHS but far fewer of them. Their main function will be as specialists to treat complex cases on a secondary – and more likely – tertiary referral basis. Will the public care or even notice the difference? I honestly doubt it. One person sitting at a desk in a consulting room with a stethoscope draped around their neck looks pretty much like another whether registered medical practitioner, PA, ACP or whatever.
I further foresee an expanded network of private clinics outside the NHS staffed very largely by “traditional” doctors offering (what will be advertised as) a “Rolls Royce” service for those well off enough to afford it, most probably those with health insurance likely funded in many cases by their employer. I can also foresee this expanded private sector and those with health insurance – and those who provide it - being granted significant tax concessions to encourage take up. In essence, we will be left with exactly the sort of two-tier health system that the NHS was originally set up to eradicate.
So who are these non-doctors who will replace the traditional registered medical practitioner? What they are not, what they do not have is the traditional undergraduate training at medical school and several years of further training as a postgraduate. Such individuals either undertake a much curtailed course of training as compared to that given in a traditional medical school or they migrate from an associated discipline such as nursing or physiotherapy. Crucially, they exist outwith the traditional hierarchy of the medical profession and its power structure. The medical profession has no power over them. They are entirely under the control of, and essentially owned by, their employer – the employing health authority and ultimately the government. Which suits the government perfectly.
The argument of the medical profession is that these “non-doctors” are fundamentally dangerous to patients because they are inadequately trained. The BMA has published many reports citing examples of patients who have suffered at the hands of these non-doctors. Of course, “proper doctors” may make mistakes as well. To play devil’s advocate it should be pointed out that the BMA and the medical profession do not have, to the best of my knowledge, any hard, substantive evidence that doctor substitution by PAs, ACPs or whatever actually does provide an inferior service to patients. In other words there are no randomised controlled trials comparing outcomes between the two groups. If the medical profession did have the benefit of a proper scientific analysis showing that traditional doctors produce significantly better outcomes for patients then its argument that doctor substitution is dangerous would be unassailable. It is puzzling to me why the profession does not demand such an analysis or even organise the study itself.
What published work there is comparing doctors with PAs and ACPs is largely observational and of restricted value in any event because analysis of outcomes between the two groups is often not based on strictly comparable groups of patients. But the conclusions – for what they are worth – are that in terms of outcomes and patient satisfaction there is little to choose between the two groups. I really do believe there is urgency to organise proper RCTs to establish the real effect of doctor substitutions on patient outcomes – and costs – once and for all.
Should the changes to health care provision described above be realised the medical profession is going to have adapt to them. Quite how it is going to do so I cannot imagine. Chaos is a much overused word in the modern lexicon but I think the chaos is likely to be the best description of the state of the profession during the transition. The profession has been effectively rudderless and leaderless for many decades past. It will have to pull itself together - and the Royal Colleges in particular – will have to show a degree of leadership, strategy, solidarity and common sense which has been noticeably lacking on their part during my own long professional career.
When the dust has settled there will probably be fewer doctors as such overall, largely employed or self employed in the private sector. Some of them will do sessions in the NHS – or what is left of it – and there may still be a few specialists wholly employed in the NHS. One of the strategic mistakes which I believe the resident doctors have made in their present dispute is making the issue about poor pay. Paradoxically the system of UK healthcare which I foresee will lead to doctors’ incomes being considerably greater than today.
So, where does all this leave us? How likely is this speculation to be realised? In the last resort, time alone will tell. All I would say, in conclusion, is that – in making predictions in good faith – it should not be assumed that the predictions represent the desired outcome. For my part they do not. My personal belief is that Bevan got it right in 1948 and his is that model of health service we should stick to. But, as another great statesman once pointed out, when the tides and currents of history are flowing in a certain direction, you cannot resist them. And I believe that’s pretty much where we are today.
William Hayes-Wood
December 2025